The agency released medical records, saying the vehicle scene was a lawful continuation of hospital care.
Medical professionals have warned that finishing an injection outside a medical facility can be legally problematic.
The episode has reopened questions about medical practice for celebrities and exposed gaps in the system.
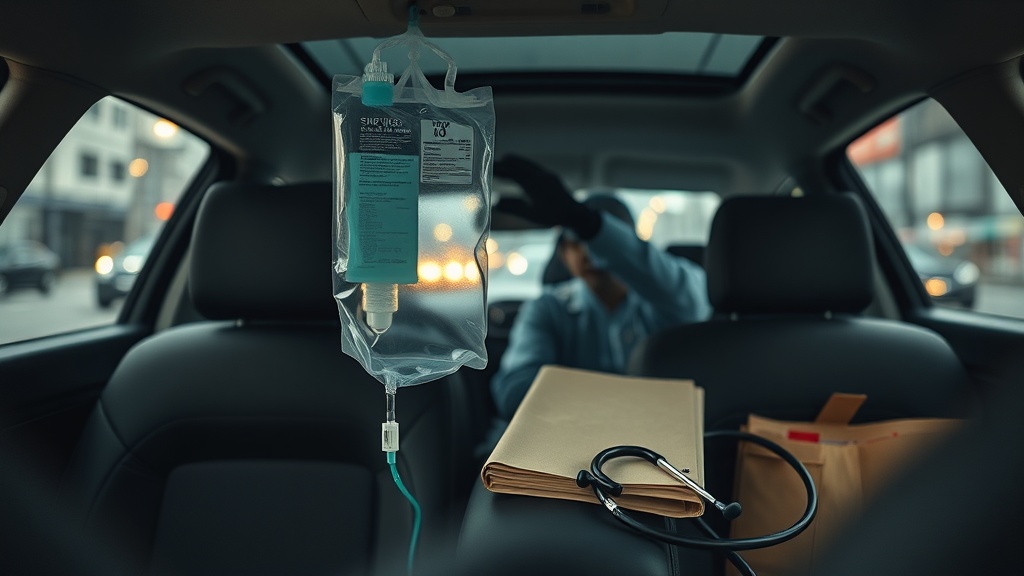
Jeon Hyun-moo IV Drip: Legal?
Overview and the Main Question
The case returned to public attention.
A clip from the 2016 episode of MBC's I Live Alone (a Korean reality show) showing an IV being administered in a car circulated online after a separate 2025 scandal involving illegal injections. Following that, someone filed a complaint through a public government portal called Gukmin Sinmungo, prompting the Gangnam Police Station in Seoul to open an investigation into whether medical law was violated.
The central legal question is whether finishing IV-related steps in a car—after diagnosis, prescription, and initial insertion took place in a hospital—counts as unlawful medical practice outside a licensed facility.
Completing injection-related tasks outside a medical facility raises serious legal concerns.
Timeline
Medical records exist.
Jeon Hyun-moo reportedly visited a hospital on January 14, 20 and 26, 2016, receiving formal diagnoses and IV prescriptions for bronchitis and related conditions. The released records show physicians made the decisions and prescribed fluids. The broadcast included a scene in which, due to a tight schedule, an IV infusion was shown being finished in a car.
After the 2025 controversy over another entertainer, the old clip spread online and a complainant filed a report. Police then began fact-finding, focusing on whether any steps that should have been done inside a facility were carried out outside one.
Agency Statement
The explanation is straightforward.
SM C&C released the medical records and says the hospital prescribed and started the infusion, and that finishing the process in the car was done under medical judgment as part of continuous care. The agency also says medical waste was collected by the hospital later, and that there was no intent to break the law. It added it will cooperate fully with the investigation.
In short, the agency insists this was an extension of lawful treatment, not an illegal act.
The agency repeatedly emphasizes this was a lawful extension of clinical care.
Key Legal Issues
The standard is the Medical Service Act (medical law).
The debate centers on whether steps such as inserting or removing needles, disinfecting the site, and handling medical waste must be performed only by licensed medical personnel inside a licensed medical institution. Courts and investigators will look at the statutory definition of medical practice, the legal meaning of a medical institution, and who actually performed each task.
Another legal wrinkle is the statute of limitations. Under current interpretation, alleged violations of medical law can have a 5-year limitation period, so whether the conduct falls within that window will affect prosecutability.
Argument: It Was Illegal
Principles generally forbid it.
The established view in the medical community is that injection-related procedures outside a hospital are normally impermissible. From a clinical standpoint, inserting and removing needles require measures to prevent infection and to manage safety; doing those steps in nonclinical settings raises added risks.
If anyone removed the needle, cleaned the site, or disposed of contaminated items in the car without proper medical supervision and protocols, that could strongly suggest a breach of medical law.
Moreover, there is a fairness concern.
If celebrities receive out-of-hospital treatment that ordinary patients would not be allowed, that raises equity issues. Extended, special handling for public figures could discourage ordinary patients from seeking care or undermine standards of practice. Medical bodies emphasize public health responsibilities and warn that allowing exceptions risks abuse.
Finishing injections outside a hospital is hard to justify as an exception.
Some legal observers say investigators should question the medical personnel involved. The complaint requests inquiries into medical staff and others connected to the event; that reflects a focus on who performed the care and who bears responsibility. Professional guidance and official medical positions are likely to matter in the investigation.
Argument: A Lawful Extension of Care
Viewed as continuous care.
Jeon Hyun-moo's side argues the hospital staff made the diagnosis and inserted the IV, and that completing the infusion in the car was a judgment call by the clinicians under the circumstances. The existence of contemporaneous medical records and the hospital's later collection of medical waste are cited as supporting evidence.
Importantly, the patient followed medical instructions. Absent criminal intent, the argument says, there is no basis to treat the patient as having committed a crime.
The statute of limitations is a key defensive point.
Because the alleged conduct took place in 2016 and the statute of limitations for many medical-law offenses is interpreted as five years, some legal analysts say prosecuting now would be difficult. In practice, the risk of criminal punishment for the patient is considered low; any inquiry is more likely to focus on the medical staff and institutional procedures. Thus, limitation periods and evidentiary issues are central to predicted outcomes.
There is also a practical perspective.
Entertainment professionals often have packed schedules that make long hospital stays impossible. In such settings, medical teams may take interim steps to protect a patient's health. If the law were read to ban all such accommodations categorically, the healthcare system would need workable alternatives that protect safety without penalizing necessary, pragmatic care. Advocates of this view call for clear guidelines rather than blanket condemnation.
Social Impact and Policy Implications
The debate spreads beyond scandal.
This case raises broader questions about the boundary between medical safety and the realities of certain professions. If rules on exceptions are unclear, similar incidents can recur. Therefore, regulators should consider clarifying what exceptions, if any, are permissible and under what documentation standards.
In practice, better written policies, explicit exception criteria, and stricter record-keeping would reduce disputes.
Meanwhile, media and the public should focus on verified facts. Overheated speculation and personal attacks do not substitute for legal and medical inquiry. Objective evidence—medical charts, staff statements, and waste-handling receipts—must guide judgment.

Investigation Outlook and Practical Steps
Evidence will decide the case.
The police will check medical records, hospital testimony, and documentation of medical-waste handling. Who did what, when, and where will determine legal findings. The statute of limitations issue will also be reviewed by prosecutors if charges are considered.
On the practical side, hospitals need clear internal rules on the limits of emergency or interim care and how to document decisions. If staff allow a patient to leave before all steps are completed, that decision and the allocation of responsibility should be recorded. Clear protocols reduce legal ambiguity and protect both patients and clinicians.
Comparisons Abroad
Other countries offer perspective.
In many places with developed emergency systems, nonprofessional injection procedures outside formal care are explicitly restricted. Ambulance services or licensed clinicians usually handle injections, and the rules about liability are strict. By contrast, some systems that support home nursing or telemedicine allow certain clinician-directed in-home procedures under defined conditions.
In Korea's context, the lesson is that the rules need to be clearer. Society must decide how to balance occupational realities, patient rights, and clinician responsibility. A transparent public debate can help set consistent standards.
Recommendations
There are practical fixes.
First, medical institutions should adopt clear internal guidelines that protect continuity of care and patient safety. Second, any exception to usual practice must be documented in writing, with clinician approval and informed patient consent. Third, public agencies should consider drafting temporary guidance for professions with extreme scheduling pressures, like entertainers, to ensure equal treatment and safety.
Finally, journalists and civic actors must prioritize fact-checking and avoid personal attacks. Legal findings should follow investigative and court processes to ensure fairness.
Conclusion
Norms and evidence matter.
This dispute highlights legal boundaries for out-of-hospital care, clinician responsibility, and limitations periods. Both the medical community's concern and the agency's explanations carry weight. The investigation should reveal the facts, and the broader lesson is clear: stronger rules and better documentation are urgently needed to prevent future conflicts.
Public debate should now focus on policy changes rather than only assigning blame. What matters next is what reforms follow.